Blog, News & Offers
Diabetes and sight loss
Posted on Tuesday, February 16, 2021
Diabetes is one of the leading causes of preventable sight loss in the UK. By recognising the signs of the eye conditions associated with diabetes, you can prevent future problems with your vision and eye health.
WHAT EFFECT DOES DIABETES HAVE ON YOUR EYES?
The changes in your blood sugar levels, caused by diabetes, can often affect many parts of your body and how you feel, this includes the lens inside your eye. Changes in your blood sugar levels can make your vision blurry, this can change throughout the day and even day to day as your levels fluctuate.
If recently diagnosed as diabetic or recently started treatment we may decline performing a sight test as these changes in the eyes lens can produce a spectacle prescription on the day which may have changed by the time you come to collect your new specs.
If you have diabetes, you might also be at higher risk of certain eye conditions when compared to others without diabetes; this can include cataracts, glaucoma and retinopathy.
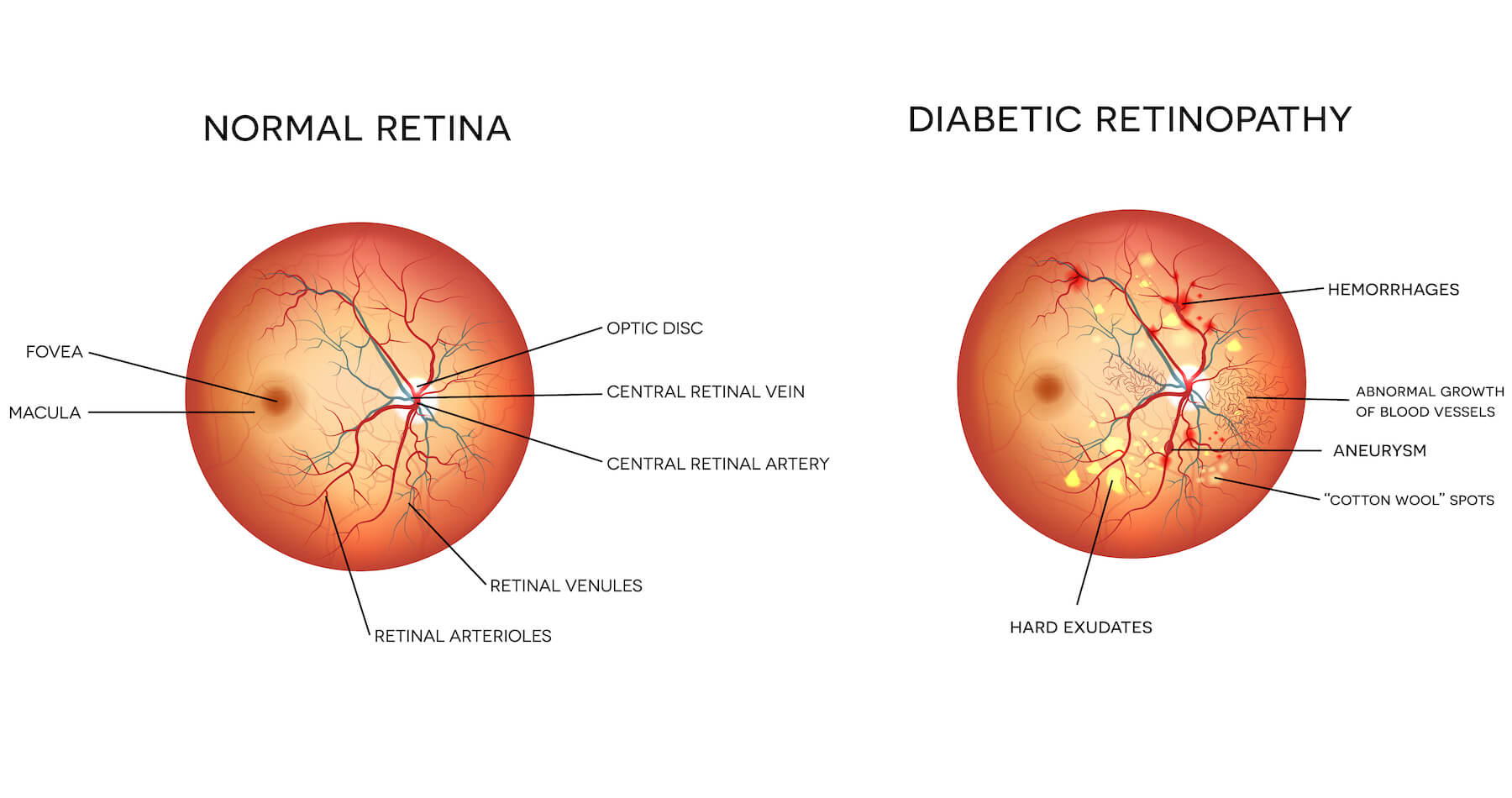
DIABETIC RETINOPATHY
Diabetic retinopathy is directly related to diabetes and occurs when there is damage to the blood vessels in the eye. Over time, diabetes can affect the blood vessels supplying the retina of your eye due to high blood sugar levels, affecting how it works. There are different types of retinopathy, with each type progressing in stages. There are many signs we look for during assessment of the eye. Some of these are shown on the photo above and include; Haemorrhages (leaked blood vessels), Abnormal growth of blood vessels (similar to AMD, can burst leaking fluid), Aneurism (bulge of blood in weak wall of blood vessel, can leak), Cotton wool spots (Damage to the nerve fibre layers) and Hard exudates (blockage causing fats and proteins to leak into retina). Someone with diabetic retinopathy may have a combination of the above clinical signs present with varying effects on their vison.
Diabetic retinopathy doesn’t usually present noticeable symptoms because the condition is gradual. If you have had diabetes for a long time, or your blood sugar levels and blood pressure are high, you can be at higher risk.
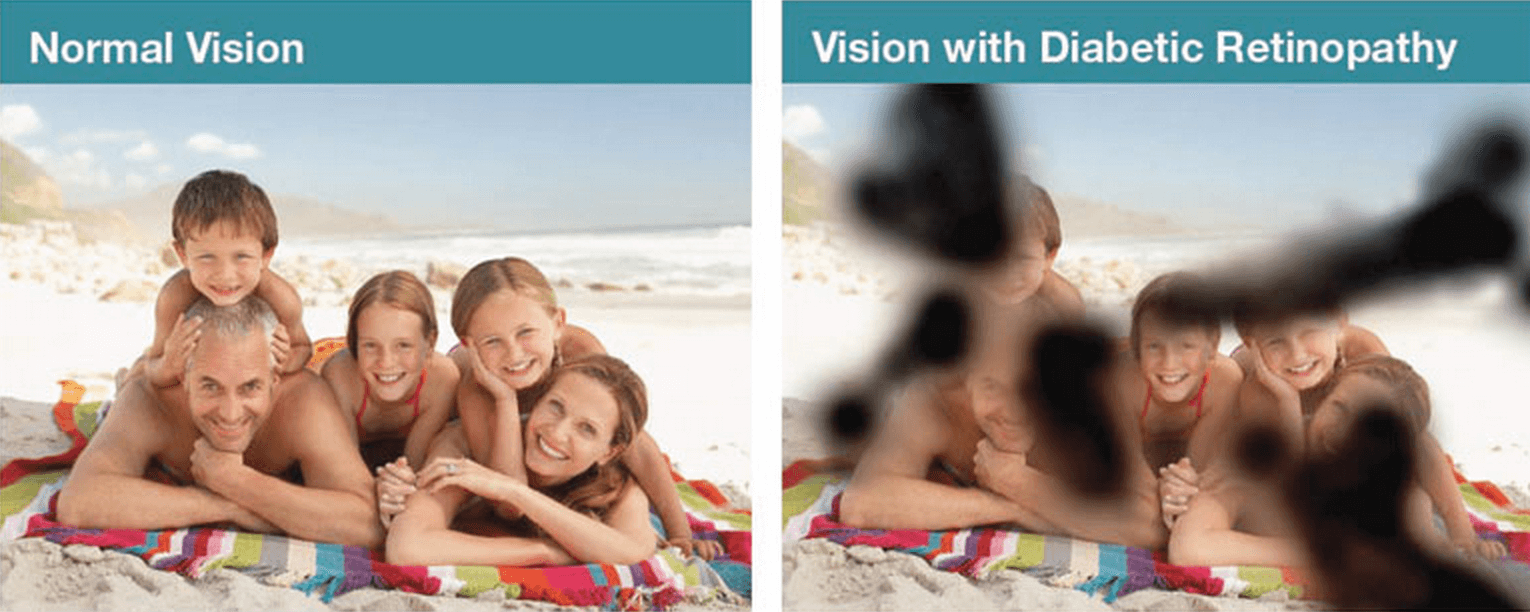
The effects noticed will be of sporadic patches missing in a personal visual field or peripheral vision. If central vision is effected they would have Diabetic Maculopathy as it effects the central Macular rather than peripheral retina.
The picture above is an example of how someone with a few areas effected in their eyes might see.
Treatment is available for diabetic retinopathy, with several different options depending on which stage the condition has reached. Your eye care professional will be able to advise on a case by case basis. These include laser treatments to contain damage within a “wall” created by a laser to injections into the eye similar to those for AMD.
In all cases, the better the diabetes is managed the better the outcome on vision is likely to be.
CATARACTS AND DIABETES
Cataracts are a common eye condition in people aged 65 or over and usually develop gradually over the years. As diabetes can affect the lens of your eye, being diabetic can increase your chances of developing cataracts. You may find that you contract cataracts at an earlier age than expected.
When you have cataracts, the lens in your eye gradually becomes cloudy and impairs your vision. It is not painful, but it can cause symptoms like blurry vision, faded colours, double vision, or seeing a halo effect when looking at lights.
You can undergo cataract surgery to fix this, which is a very straightforward operation. It is one of the most common procedures in the UK.
GLAUCOMA AND DIABETES
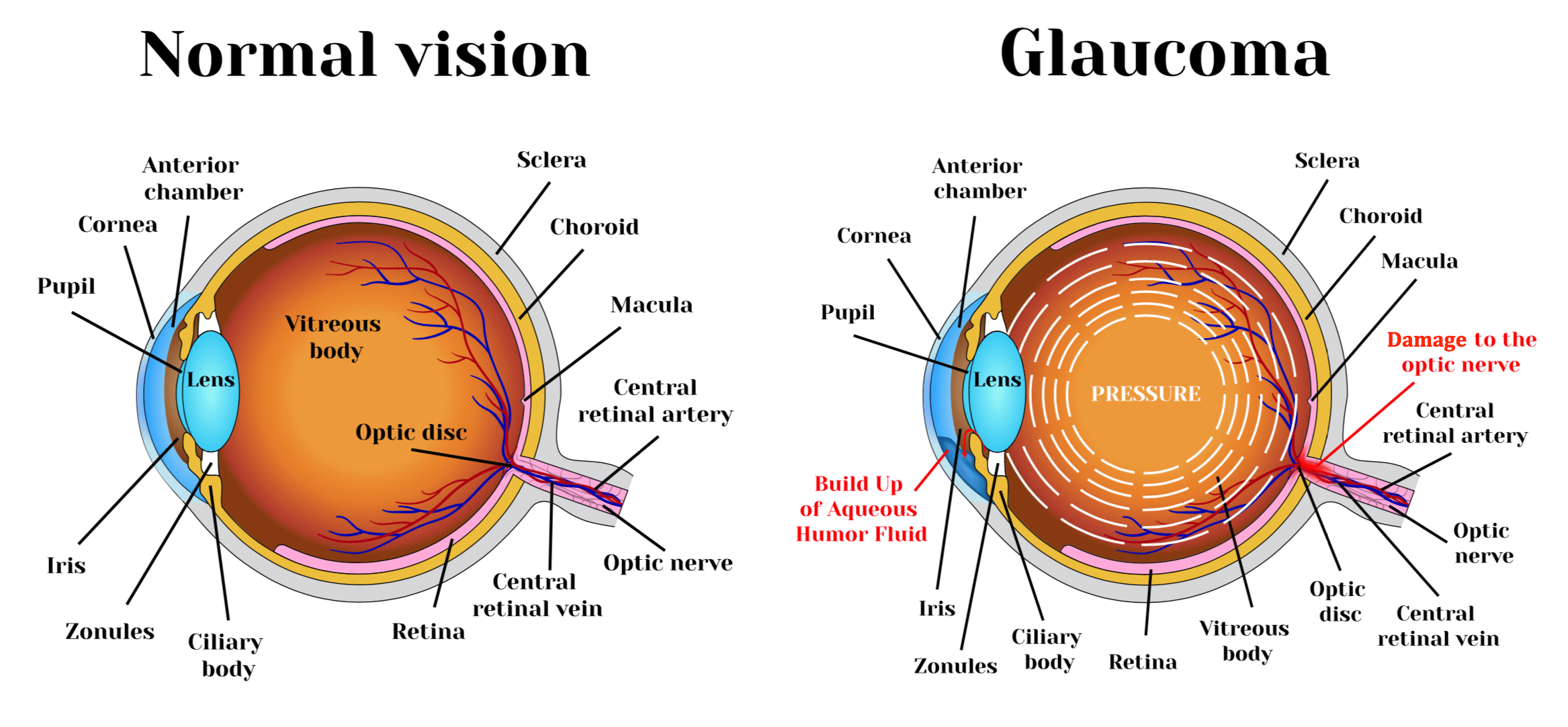
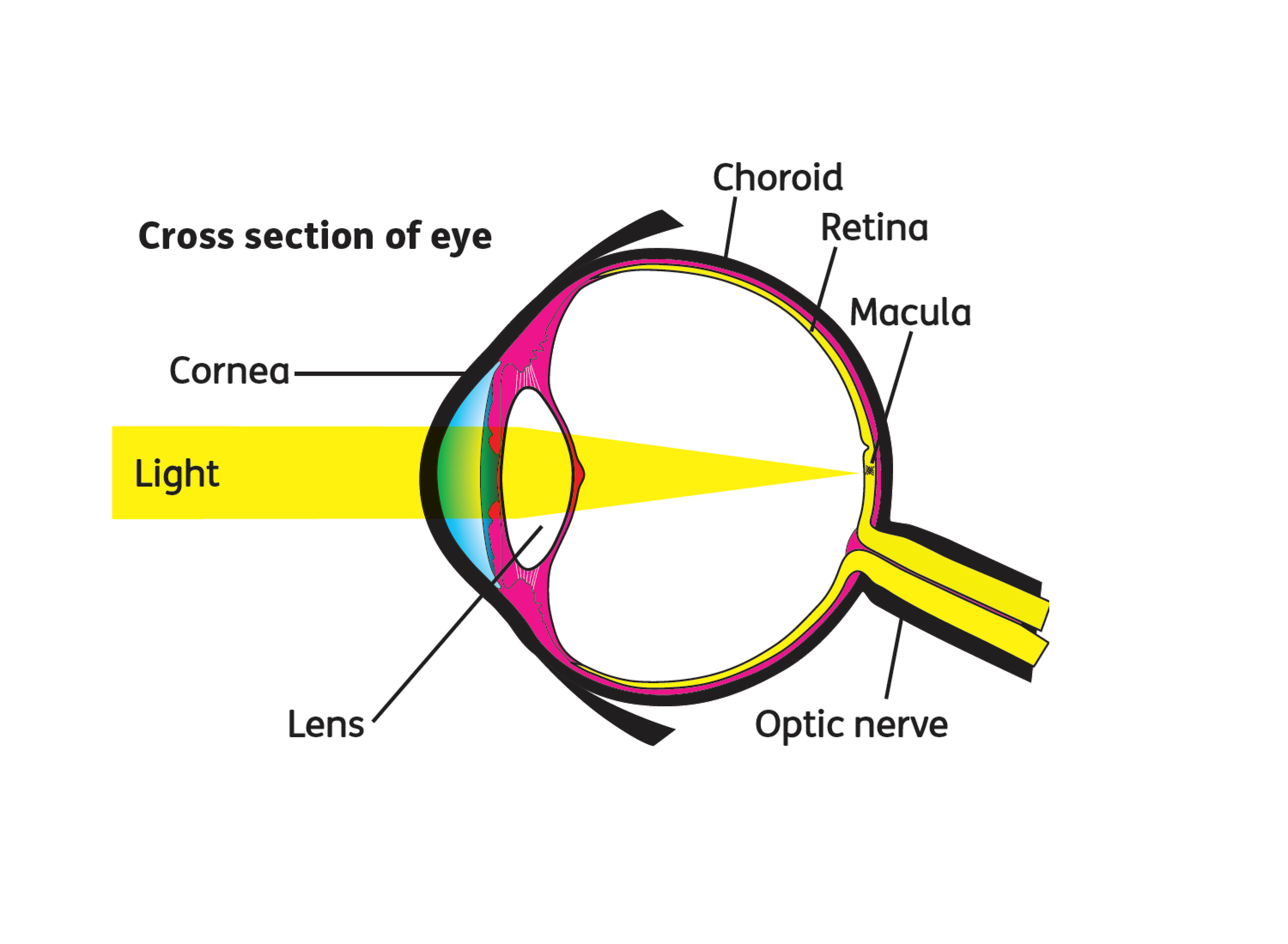
If you have diabetes, you may be more likely to develop glaucoma. Glaucoma happens when there is a build-up of pressure in the eye, which can lead to damage around the retina or optic nerve if not treated.
Symptoms of glaucoma are not always noticeable but can include eye pain, redness, headaches and misty vision. Those with diabetes have a higher risk of developing glaucoma, but it can be easily treated if found early enough. You can see our other blog for more information on Glaucoma.
REDUCING YOUR RISK OF EYE DISEASE IF YOU HAVE DIABETES
The most important thing you can do to protect your overall health is to keep your diabetes under control as best you can to reduce your risk of many different health complications, including eye diseases. You should closely monitor your blood sugar levels, blood pressure and cholesterol levels.
Maintaining a healthy weight and keeping fit is also essential to reduce your risk of eye disease. Poor diet and other similar lifestyle choices can trigger many eye conditions. Quitting smoking, or not taking up smoking in the first place, is also very important for everyone’s health but particularly if you have diabetes. Smoking can increase your blood pressure and may raise your blood sugar levels.
EYE SCREENING
If you have diabetes, the NHS offers an annual diabetic eye screening service for those aged 12 and above as well as free sight tests on either an annual or biannual basis depending on your age or health of your eyes. It is crucial that you attend regular sight test appointments as well as going to your screening, as they can detect diabetic retinopathy in your eyes before your vision is affected.
The screening DOES NOT look for any other issues with your eyes such as Glasses prescriptions, Corneal health, Macular degeneration, glaucoma and cataracts as well as many more. In a nut shell that service are only looking for diabetic changes. We are able to offer screening in our non Staffordshire practices, sadly the funding for Opticians to perform screenings in Staffordshire has ended so you will be called to a mobile screening location and given a designated date and time if you are registered with a GP in this area.
Covid 19 has had an effect on Diabetic screening creating a large backlog. The diabetic services have looked at historic data to see which patients have consistent healthy screenings and as a one off due to pandemic these patients will skip a year and be seen in 2021. Any new diabetics or people with historic issues who are being monitored more carefully will still be seen.
If you have diabetes and have noticed a change in your vision you should not wait for your screening, its most likely a change in prescription but it could be something more serious, book a free sight test to make sure.
As with all sight impacting conditions there is an ever changing landscape of low vision devices and support groups to help assist a person suffering with sight loss.
Our final blog of the month will be about the latest tech on the market that can assist someone with serious sight loss.
Low vision awareness month; Glaucoma.
Posted on Tuesday, February 9, 2021
Glaucoma, What is it and how does it effect sight?
Glaucoma is a group of eye diseases that affect the optic nerve, the nerve which connects the eye to the brain. The damage is caused by an increase in pressure inside the eye (intra ocular pressure or IOP).
It often affects both eyes, usually to varying degrees. It affects the most peripheral vision first gradually working its way to the central vision area and for that reason the effects often go unnoticed until it can be quite advanced. In most cases it is asymptomatic and is hence know as a silent blinder of sight conditions. It is treatable but best managed if detected early, something which can be done through a routine eye test.
What causes Glaucoma?
Inside the eye, a continuous production of fluid occurs called the aqueous humour. This fluid has a very important job of maintaining the shape of the eye as well as keeping the back of the eye pressed down so it can function correctly. Normally as new fluid is produced, old fluid makes its way to drainage tubes where it leaves the eye. In glaucoma this drainage is damaged or blocked somewhere along the fluids pathway causing a build up of fluid and an increase in pressure. Imagine a sink with the tap on, glaucoma is either the plug being closed or partially closed or the pipes under the sink being blocked.
There are 2 main subtypes of glaucoma, Chronic and Acute.
Chronic is the most common type which develops very slowly. It is painless and will effect the vision slowly from the outside in and therefore needs detecting through a sight test.
Acute Glaucoma is painful and has a sudden onset due to a rapid increase in IOP. The pain is usually extreme and not something you may ignore with blurred vision and halo’s around light also noticed. In this instance you should go immediately to a hospital with an eye A+E department. In our practice areas this would be Burton Queens, Birmingham City or Wolverhampton New cross hospitals.
In my earlier comparison, Chronic glaucoma is either the plug being slightly covered or the pipes being slightly blocked so the water doesn’t run away quite as efficiently, Acute is where the plug is in or the pipes are blocked so the sink fills with water and has nowhere to go.
The most common types are:
• Primary open angle glaucoma, the most common type of glaucoma in the UK. It’s also known as chronic open angle glaucoma which means the damage to your optic nerve and changes to your sight happen very slowly over time.
• Closed angle glaucoma, where damage to the optic nerve can happen very quickly due to a sudden rise in eye pressure.
• Normal tension glaucoma, when an eye pressure within the normal range still causes damage to the optic nerve.
• Secondary glaucoma, which occurs as a result of another eye condition, an injury to the eye or due to medication.
• Congenital glaucoma, when a baby is born with glaucoma.
What factors increase your risk?
Risk factors for glaucoma include:
• increasing age,
• high pressure in the eye,
• a family history of glaucoma,
• being short sighted (myopic)
• use of steroid medication.
You are also at increased risk of developing chronic glaucoma if you are of black-African or black-Caribbean origin, whereas people of Asian origin are more at risk of getting acute glaucoma compared with those from other ethnic groups.
Because Family history is such an important risk factor, anyone over the age of 40 directly related to someone with glaucoma can have NHS sight tests, either every 12 months or 2 years depending on what is found on the sight test.
Testing for glaucoma.
Eye pressure test (tonometry)
An instrument called a tonometer is used to measure the pressure inside your eye – intraocular pressure. Tonometry can be useful to identify ocular hypertension (OHT – raised pressure in the eye). In some opticians this device produces a puff of air into the eye. In all of our practices we have non puff tonometer’s.
Visual field test
By staring straight at a central light/target throughout, You will be shown a sequence of lights and asked to respond by pressing a button when you notice a light flash in your peripheral vision. If you can’t see the spots in your peripheral vision, it may indicate the glaucoma has damaged part of that area of vision.
Optic nerve assessment
Your optic nerve connects your eye to your brain. This can be assessed in a variety of ways during your examination. We are interested in the cup to disc ratio or in other words the size it is round by how deep it appears like a tea cup. Too much pressure forces to cup to become deeper.
OCT (Optical Coherence Tomography)
OCT scans are similar to MRI and ultrasound scans and can help opticians detect signs of glaucoma and other conditions up to four years earlier than more traditional imaging methods. The scan produces a 3D-like image that allows us to see the structures of your eye in even greater detail. Over time, your optician will be able to spot the changes that indicate the start of glaucoma. Ask your local store if they offer OCT and you can add it to your eye test for an additional fee.
Treatment
Glaucoma cannot be cured but in many cases it can be managed to slow the progression to avoid glaucomatous damage and nerve damage, which will preserve the visual field and provide total quality of life for patients, with minimal side-effects. Sadly however there are some people less fortunate or those with rarer strains of the condition who are left visually impaired.
Glaucoma can be treated:
• Medication; Using eye drops to either help the flow of fluid in the eye or slow its production.
• Laser; Laser can be used to create a hole allowing fluid to leave the eye or to remove a source of blockage in effect.
• Surgery; Implants can be put in to bisect a blocked area.
Low vision considerations
Ophthalmologists can refer patients with low vision caused by any eye condition to a low vision clinic where assessments can be conducted to determine if any devises can improve everyday life for someone living with an eye condition. With glaucoma the peripheral vision is damaged first leaving the central area of vision functional or partially functional.
To empathise how this would feel close one eye and look through a toilet roll tube or tube made from your fist.
Spectacle lenses are designed to focus light entering the eye as sharply as possible into the back of the eye. They unfortunately cannot be used to improve lost field of vision, only make the image as sharp as possible on the non damaged area's.
Low vision therapy can be anything from teaching someone how to use their functional areas of vision to the use of telescopes or magnifiers to ensure an image falls on the functional area of vision. Low vision aids can be quite expensive so these are loaned to patients from the hospital/social services or purchased privately direct from source.
Central vision is more sensitive to colour vision, whereas peripheral cells are more tuned to black and white so night time can be an issue as well as black and white images, filters and adequate lighting are key to successfully using functional retained/residual vision.
There are many support groups and networks for either people living with low vision or specifically glaucoma. These are excellent resources as no one can understand the challenges and how to overcome them better than someone who also has the condition. You cannot learn that form of experience through reading.
Modern technology is always producing new and exciting low vision aids, some which we couldn't have imagined possible one generation ago. If you know someone with low vision needs, there are yearly shows put on in places like the NEC where the latest tech is on show to trial and see if it may be of benefit.
Lets talk about Macular degeneration
Posted on Thursday, February 4, 2021
February is Low vision awareness month, Let's talk about Macular Degeneration
Macular degeneration is the most common cause of sight loss in people over the age of 50 in the UK. It is sometimes referred to as age-related macular degeneration or AMD or ARMD. There can be quite a bit of confusion cause about treatments for this condition especially from newspapers as there are 2 subtypes and the most common type has few treatment options.
What is the macula?
The macula is part of the retina at the back of the eye. It is only about 5mm across but is responsible for our central vision, most of our colour vision and the fine detail of what we see. The macula has a very high concentration of photoreceptor cells – the cells that detect light. They send signals to the brain, which interprets them as images. The rest of the retina processes our peripheral, or side vision.
What causes AMD?
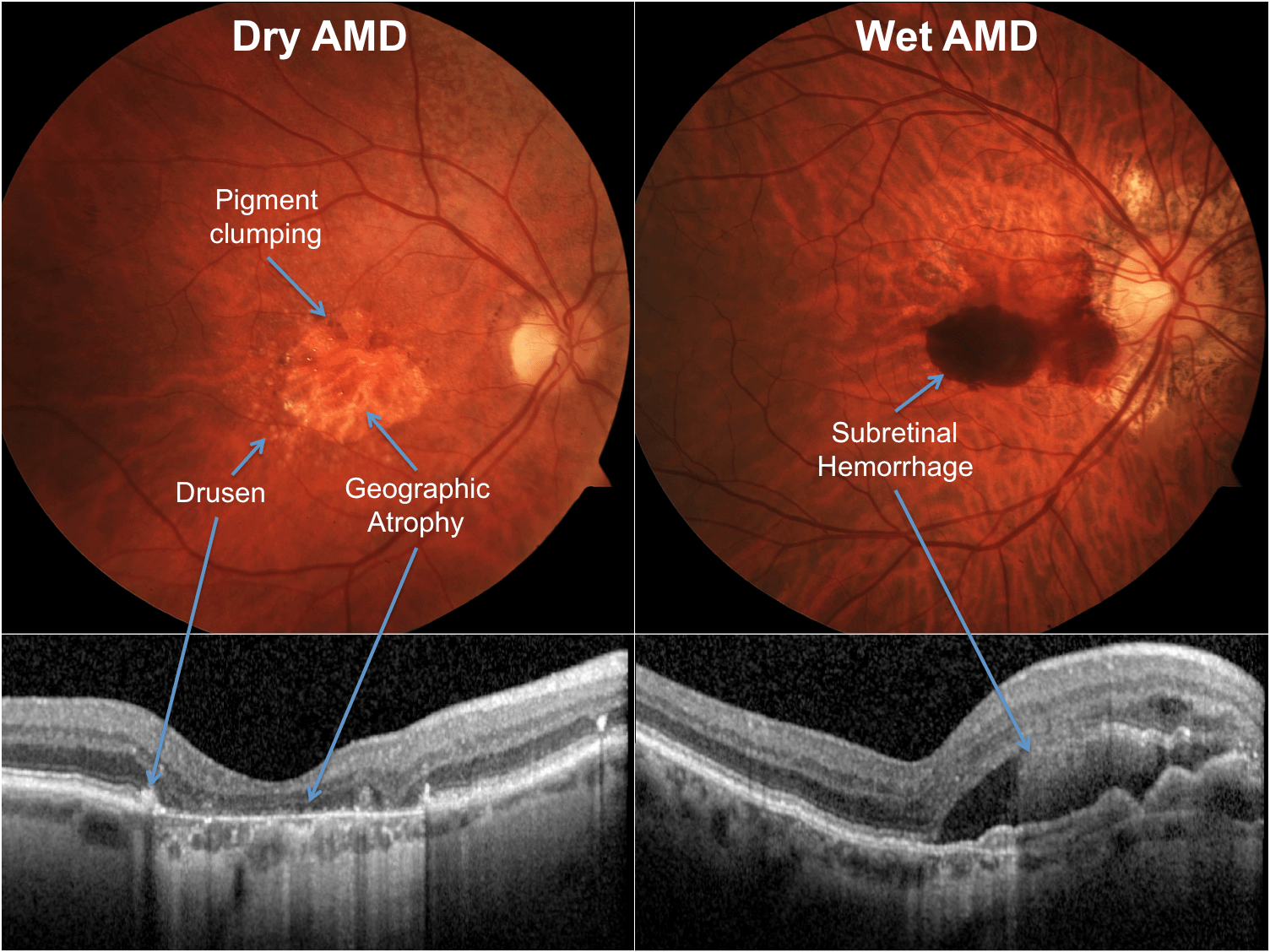
There are 2 types of macular degeneration Dry and Wet. Dry is the most common making up over 90% of cases.
Dry AMD
Dry AMD is a slow deterioration of the cells of the macula, often over many years, as the retinal cells die off and are not renewed. The term ‘dry’ does not mean the person has dry eyes, just that the condition is not wet AMD.
The progression of dry AMD varies, but people often carry on as normal for some time.
Wet AMD
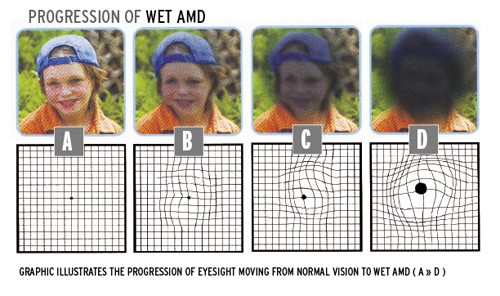
Wet age-related macular degeneration (AMD) develops when abnormal blood vessels grow into the macula. These vessels are weak and leak blood or fluid which leads to scarring of the macula and rapid loss of central vision. Wet AMD can develop very suddenly, but it can now be treated if caught quickly. Fast referral to a hospital specialist is essential.
A person with dry AMD can also develop wet AMD which is treatable, so it is important to act on changes in vision.
What are the symptoms?
The symptoms for both wet and dry AMD are similar although in wet AMD the symptoms occur quickly and are more severe with Dry occurring over a long period of time and going undetected or mistaken for general blurring of vision often assuming that a change in spectacles is needed.
The most commonly appreciated symptoms are:
• Gaps or dark spots (like a smudge on glasses) may appear in your vision, especially first thing in the morning. Objects in front of you might change shape, size or colour or seem to move or disappear.
• Colours can fade.
• You may find bright light glaring and uncomfortable or find it difficult to adapt when moving from dark to light environments.
• Words might disappear when you are reading.
• Straight lines such as door frames and lampposts may appear distorted or bent.
What causes AMD/risk factors?
• Age
• Family History of AMD
• Smoking
• Weight
• Exposure to UV (sun)
• High Blood pressure
Diagnosing AMD
AMD can be diagnosed by your Optometrist during routine or emergency sight testing.
In all sight tests we not only test for spectacle prescriptions but most importantly we look at the eyes health. There are parts of the eye which cannot be seen easily but the macular is positioned centrally so is a more easily assessed part of the eye. Sometimes however dilating eye drops are needed so that the bright light we use to view inside the eye stop your pupil from going small (the body’s normal, involuntary response to viewing bright lights)
As these changes often occur deep within the back of the eye viewing alone may not be enough to see changes occur and additional tests are needed such as OCT (Ocular coherence tomography) which can either be done at Hospital by referral or at some branches for an additional fee of £40.
OCT is also a good for providing your optometrist with a bench mark reading to look back on if changes in vision occur.
Treatment for AMD
There is no medical treatment for dry AMD, there are many research projects going on to find treatments or cures which you may read about in the news.
Several drugs are used to treat wet AMD. They are known as ‘anti-VEGF’ drugs. VEGF stands for ‘vascular endothelial growth factor’. It is the substance in the body that is responsible for the development of healthy blood vessels. In wet AMD, too much VEGF is produced in the eye, causing the growth of unwanted, unhealthy blood vessels.
Anti-VEGF drugs block the production of VEGF and stop the development of abnormal blood vessels. All the anti-VEGF drugs are given as an injection into the eye.
Lucentis® was the first anti-VEGF to be licensed for wet AMD. The normal procedure is that all patients receive a standard ‘loading dosage’ at the start of their treatment: normally three or more consecutive monthly injections. Eylea®.is another medication used but usually used for patients expected to be needing injections for longer as the interval between doses is increased and provided in non-consecutive months.
In December 2020, NICE (national institute of clinical excellence) announced that Beovu® had been approved to treat wet AMD. This new anti-VEGF treatment is longer-acting than the current treatments, and needs to be injected only around every 12 weeks. Patients who react well to the drug could have their injections spaced even further apart.
After this initial phase, there are a number of treatment regimens that an ophthalmologist can choose. Each regimen has a subtle difference in the frequency of appointments. They also vary as to whether or not you have an injection at every appointment.
Non medical treatments
Spectacles focus the light onto the macula as this is the most sensitive part of the eye, when damaged the peripheral vision becomes the most functional area of vision. Some people benefit from extra magnification for near as this makes the image falling on the back of the eye larger than the macular therefore falling on the functional part of the eye. Usually however people develop an enhanced use peripheral/eccentric fixation techniques, this technique requires someone to look away from or not directly at an object so it can be seen in their peripheral vision.
Hold out your hand and look straight at a finger, you can see the finger you are staring at in great detail. This is macula detail. While staring at the same finger notice the other fingers but do not look towards them, the detail isn’t as sharp but still functional. This is peripheral vision and falling on the retina.
There are now spectacles that force the image to fall onto a person’s best area of peripheral vision for them by looking straight ahead.
The peripheral area of the back of the eye is more sensitive to black and white vision rather than anything with colour. Yellow tints on spectacles can help to reduce colour perception and encourage black and white vision. For the same reason it is best that devices used around the house settings are adjusted to black and white mode like phones and televisions.
Making objects bigger can also help (magnification). Eg television; This can be done by moving televisions closer, investing in a bigger screen or by using low vision aids like magnifiers. The same principle applies to other objects.
There are many other low vision aids that can assist a person with sight loss for all manner of tasks such as whistles to alert you when pouring a cup of tea and stickers that can be applied to a cooker for finding popular heat settings. These can be purchased privately or available through low vision clinics.
An Ophthalmologist can refer patients to low vision clinics where expensive magnifiers and low vision aids can be loaned out to people after proper assessment to determine which powers or techniques will suit a person best.
There are also many support groups such as macular society as well as local support groups where people can share their experiences and assist people with suggestions.
Our dispensing opticians at every practice are trained in assisting patients learning eccentric or peripheral viewing techniques. The area which is best for each person is unique to them so must be found by trial and error. There are some things we can do with spectacles but we unfortunately will not be able to provide the improvements people desire from memory of corrected sight with glasses.
I hope this blog will be useful and if there is one takeaway point I would say is act quickly if you or someone you know mentions a loss in vision, swift action can lead to a better prognosis. We are open throughout the covid pandemic and beyond providing emergency and routine sight tests.
Special delivery! We will deliver your solutions
Posted on Wednesday, February 3, 2021

Are you one of the thousands of patients who use wetting drops for dry eye conditions?
If so we are happy to deliver these products to you.
We stock many different products including Theloz, Hyabak, Hycosan, Systane, Blepha Range, Viscotears, Tears natural and eye mist spray.
We are also able to supply anti-fog, cleaning and contact lens solutions.
Free delivery on orders over £20. Call your local practice and they will be able to take payment over the phone and get them sent out to you.
Blog Search
Blog Categories
- News & Offers (50)
Blog Archives
- August2023 (1)
- April2023 (1)
- November2022 (1)
- October2022 (2)
- September2022 (1)
- August2022 (3)
- June2022 (3)
- May2022 (3)
- March2022 (3)
- December2021 (2)
- November2021 (1)
- June2021 (1)
- May2021 (1)
- April2021 (2)
- March2021 (2)
- February2021 (4)
- January2021 (1)
- December2020 (1)
- November2020 (2)
- October2020 (1)
- September2020 (3)
- July2020 (1)
- April2020 (2)
- March2020 (2)
- October2019 (1)
- July2019 (2)
- June2019 (1)
- February2019 (1)
- January2019 (1)